- Free First Class Delivery
- Buyer Protection
- Secure Online Shopping
- Healthcare Professional? Click here
Achilles tendonitis


Categories
What is achilles tendonitis and how does it develop?
Your Achilles tendon is the band that connect the calf muscle to your heel bone. Achilles tendonitis is usually accompanied by pain associated with Achilles tendon or the bursa associated with it. It normally develops following overstrain of the tendon, such as training too hard, particularly during contact sports or sports involving burst of movement, such as running, tennis, squash, and so on.
It’s not only athletes but also overweight people who also have problems with the Achilles tendon. Rheumatism and foot deformities can also be factors the condition.
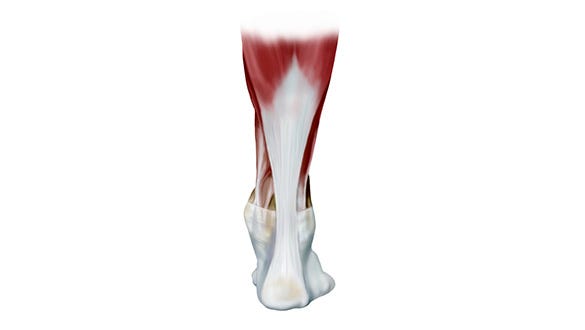
Anatomy
As the strongest tendon in the human body, the Achilles tendon transmits the power of the calf muscle to the foot movement. This facilitates the toe off motion of the foot when walking and running. When you run, a force equal to eight times your own body weight acts on the Achilles tendon.*
Risk factors and causes
The risk factors are diverse and not always straightforward.
Sporting activities
- Sprint running and jumping excessively
- Unusual stresses, for example, cross-country running
- Inadequate fitness level – over-doing it


External factors
- Unsuitable or incorrect footwear
- Smoking
- Taking certain antibiotics can cause weakened ligaments
Anatomical factors
- Wear and tear of the tendon with age
- Foot deformities
- Shortened tendons or muscles
- Elevated uric acid levels
- Rheumatic diseases
- Being overweight
Signs and symptoms
The symptoms are often pain or a mild ache in the back of the leg or above the heel after exercise, increased warmth and tenderness to touch, stiffness which improves with mild activity, and swelling around the Achilles tendon area.
Initially the symptoms only occur when starting exercise and disappear again once you have warmed up. In the advanced state of the condition, pain and swelling remains.
Treatment
Initial treatment is normally conservative, i.e. without surgery. The sooner the treatment starts, the more successful it is. The following methods have been proven to relieve pain and to slow or even stop progression.
- Physiotherapy: specific exercises** can promote reorganisation of the tendon tissue. We recommend doing the exercises to strengthen the Achilles tendon and the leg muscles for several minutes twice daily. Depending on the findings and the phase of the condition, your therapist can recommend further physiotherapy (therapeutic ultrasound), electrotherapy (TENS), transverse friction (special massage of the affected muscle or tendon fibres), shockwave therapy or acupuncture.
- Supports: special medical supports (for example Achimed from medi) can relieve the stress and strain on the Achilles tendon. The compressive knitted fabric and the integrated silicone pad, exerts a gentle massage effect on the Achilles tendon, promoting good blood circulation to the surrounding tissues. This relieves irritation and pain. In the acute phase, patients can relieve their Achilles tendon further still with separate heel wedges that are worn in both shoes.
- Insoles: orthopaedic shoe insoles can correct the body's posture and relieve tension on the Achilles tendon.
- Cold: mild cold treatments with cold packs relieve pain and swelling (refrigerator temperatures of about 7°).
- Heat: a heat pad, a hot water bottle or massage with a warm towel roll (towel immersed in warm water) can also promote good circulation around the tendon.
- Medication: depending on the need and on the doctor’s decision, affected patients maybe prescribed anti-inflammatory medication for one to two weeks.
- Ointments: anti-inflammatory creams or ointments can be massaged into the affected area several times a day. This can also promote recovery.
Central physiotherapy exercise
Eccentric training** is an effective conservative treatment method for Achilles tendonitis. This has been shown by various studies.*** Calf raises are considered the central exercise. (link down to the exercise description)
The exercise should be performed twice a day for a period of at least 12 weeks.
The exercise can be done very simply on a step (e.g. stairs) and does not require any other fitness equipment.
Important to know:
Pain in the calf muscles is to be expected during the first two weeks of performing the exercises but have patience and conscientiously continue with them. If the pain becomes too severe, reduce the number of sets. If this doesn’t help reduce the pain or if you also have pain during your day-to-day activities, stop the exercises and consult the doctor or physiotherapist.
All-in-one physiotherapy programme for achillodynia
Besides the central exercise calf raises, further additional exercises can be done to strengthen the Achilles tendon. medi has joined Dr Matthias Marquardt, sports doctor and active sportsman, to compile a training programme for this. The exercises can be done very easily at home. In the videos, Dr Matthias Marquardt teams up with the professional triathlete and physiotherapist Laura Philipp to show how the exercises are done correctly - ideally three to four times a week.
Please ask your doctor first, whether the exercises are suitable for you.
Coordination - standing on one leg
Equipment:
- Stabilisation pad (alternatively: rolled-up towel, folded exercise mat)
Starting position:
- Stand on one leg, barefoot and upright, on the stabilisation pad
- Keep the knee of the leg you are standing on slightly bent
- Lift the other leg up (one-leg stance) (Fig. 1)
Exercise:
- The soft surface of the stabilisation pad creates instability - try to constantly compensate for this
- This automatically activates your foot and hip muscles
- Please make sure your trunk muscles are tensed and that you maintain an upright posture
- To do this tense your abdominal muscles and make yourself as tall as possible
Variations:
- Make the exercise easier by doing it on a hard surface (without the stabilisation pad)
- Make it more difficult by drawing figures of 8 (with the free leg) (Fig. 2)
- Make it more difficult by lifting the free leg up to the hip (Fig. 3)
- Make it more difficult by closing your eyes
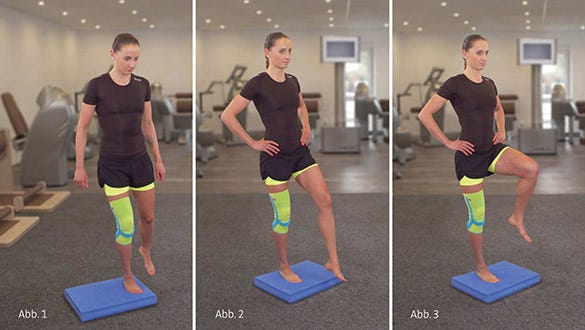
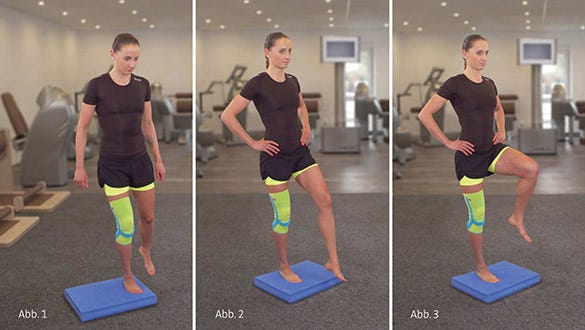
Dosing:
- Three sets per leg, hold for 30 seconds in each case
- Take a 15 second break between each set
Strengthening
Calf raises with straight knee
Equipment / Exercise location:
- A stair tread (optionally with a handrail at the side)
Starting position:
- Stand with the balls of your feet on the edge of a step
- Your heels are suspended freely in the air
Exercise:
- Keep your knees straight and stand on tiptoe
- Lift the healthy leg up (Fig. 1)
- Slowly lower the affected heel to below the level of the edge of the step (Fig. 2)
- Now lift yourself up back to the starting position
- keep your upper body upright
- do not allow the affected leg to bend inwards (no knock-kneed position)




Variation:
- Do the exercise with straight knees
- Make the exercise more difficult by adding extra weight (e.g. a rucksack with weights)
Dosing:
- 3 sets with 15 repeats per set
- Take a 15 second break between each set
Calf raises with bent knee
Equipment / Exercise location:
- A stair tread (optionally with a handrail at the side)
Starting position:
- Stand with the balls of your feet on the edge of a step
- Your heels are suspended freely in the air
Exercise:
- With your knees bent, stand on tiptoe (knee flexion approx. 60°)
- Lift the healthy leg up (Fig. 1)
- Slowly lower the affected heel to below the level of the edge of the step (Fig. 2)
- Now lift yourself up back to the starting position
- keep your upper body upright
- do not allow the affected leg to bend inwards (no knock-knee position)
Variation:
- Do the exercise with straight knees
- Make the exercise more difficult by adding extra weight (e.g. a rucksack with weights)


Dosing:
- 3 sets with 15 repeats per set
- Take a 15 second break between each set
Stretching - Calf rolling
Equipment:
- Fascia roller (e.g. from Blackroll®)
- Optional: exercise mat
Starting position:
- Sit on the floor
- Lift one foot and lay the calf of the other leg on the fascia roller
- Lean back on your hands (Fig. 1)
Exercise:
- Lift your bottom a little off the floor.
- Now slowly roll over the whole length of your calf, forwards and backwards, i.e. from the Achilles tendon to the hollow of the knee.
- You will now feel the pressure point treatment in your calf muscles.
- Your trunk muscles support thereby the movement of your body (Fig. 2).
- Point your toes downwards, so that your calf muscles are relaxed.
- The exercise may be slightly painful at first, but the pain should never be more than you can easily tolerate.
Variations:
- Make the exercise more difficult by rolling both legs
- Make the exercise more difficult by crossing your legs


Dosing:
- 3 sets with 10 repeats per set (roll forwards and backwards for each leg for the single-legged variant)
- Take a 30 second break between each set
More information
*Klein, C.: Orthopädie für Patienten [Orthopaedics for Patients]. Publisher: Michels-Klein, Remagen 2014
**Eccentric training means loading a muscle or a tendon by slowing down a weight or resistance.
***Alfredson H et al. Am J Sports Med 1998;26(3):360-366.
Visnes H, Bahr R. Br J Sports Med 2007;41(4):217-223.
O’Neill S et al. Int J Sports Phys Ther 2015;10(4):552-562.