- Free First Class Delivery
- Buyer Protection
- Secure Online Shopping
- Healthcare Professional? Click here
Patellar tendinopathy
(Runner's knee)


Categories
Patella tendinopathy is often known as jumper’s knee or patellar tendonitis. It can be caused by wear and tear or when the patellar tendon becomes irritated by unaccustomed or excessive tension forces. The injury commonly occurs during sports that involve jumping, such as basketball, netball or volleyball and also from activities that involve sudden stop-and-go movements (tennis, badminton) or quick changes in direction (football).
It is also widespread among runners where the pain is felt around the tip of the kneecap.
What is patellar tendinopathy and how does it start?
The following synonyms are used for patellar tendinopathy:
- Patella tendonitis
- Runner's knee
- Jumper's knee
Anatomy of the knee joint
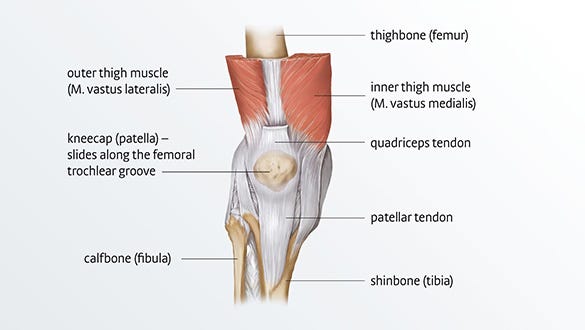
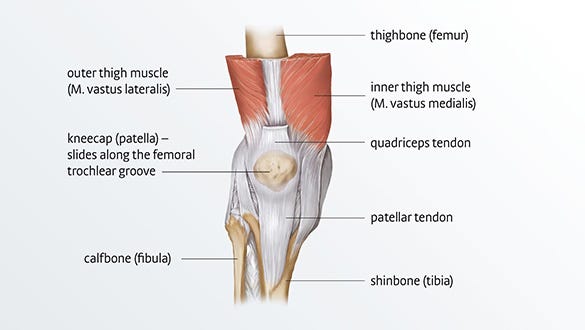
The knee joint is one of the most used joints in the human body. The thigh bone (femur), the shinbone (tibia) and the kneecap (patella) form the bony elements of the joint.
The patellar tendon (patellar ligament) is located just below the knee cap (patella). It attaches the patella to the tibia (shinbone). Its main function is to transmit forces from the quadricep thigh muscles to the lower leg and acts like a pulley as your leg straightens.
Risk factors and causes
Anatomical factors
- The elasticity of the tendons diminishes with and suffers from wear and tear
- Malalignment of the knee
- Foot deformities
- Shortened tendons or muscles
- Anatomical anomalies, for example bowlegs, knock knees or a movement disorder (dysmetria)
- Congenital ligamentous weakness (lax ligaments)
- A previous history of Osgood-Schlatter disease, a painful condition of the knee joint at the level of the shin bone
External factors
- Unsuitable footwear
- Wrong sporting techniques
- Excessively hard surfaces, for example asphalt
- Excessively intensive training sessions
- Unusual stress, for example when learning a new sport or when training is started too enthusiastically, and the knee is then subjected to extreme forces
Sports
- Sports that involve intensive jumping – volleyball, basketball, some disciplines in light athletics such as long jump or high jump – which is how it got its name, jumper's knee
- Jogging or track and field running – which is why it is also called runner's knee
- Sports with rapid changes of direction – skiing, football
- Sports with abrupt stop-and-go movements – tennis, squash, badminton
The various degrees of severity of the patella tendinopathy syndrome
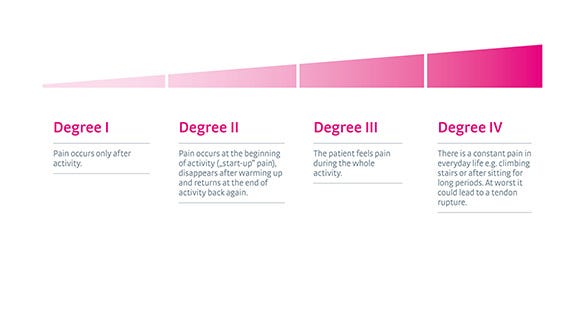
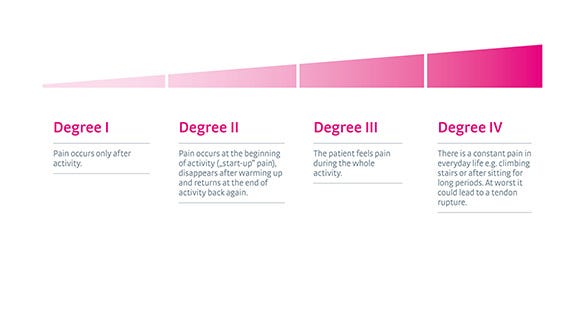
Doctors do not usually refer to the 4 stages or degrees of patella tendinopathy. This four-part classification is to help patients understand the clinical picture.
- Anterior knee pain over the tip of the knee cap
- Pain made worse with jumping, landing or running activity
- Pain is sometimes made worse with prolonged sitting
- Onset of pain is usually gradual and commonly related to an increase in sport activity
- Localised tenderness over the knee cap
- Often the tendon feels very stiff first thing in the morning


How patellar tendinopathy is treated
Patellar tendinopathy is usually treated conservatively, i.e. without an operation. Surgical intervention is only needed if the patellar ligament ruptures. The following methods can relieve pain and often stop progression.
Physiotherapy exercises
Strengthening exercises increase muscle tone and mobility. They can also boost the healing process. A doctor can refer you to see a physiotherapist. Depending on the findings, ultrasound treatment, electrotherapy (TENS), transverse friction (a special form of massage of the affected muscle and tendon fibres), shockwave therapy or manual therapy may be included as part of your therapy.
Streching
Regular stretching of the muscles over the front of the thigh reduces the tension on the kneecap.
Soft supports
Special medical supports stabilise the knee joint. Knee supports with a strap system, such as medi's Genumedi PSS, are particularly suitable for a specific reduction of the peak pressure and tension forces that act on the patellar ligament.
Cooling
Cold packs can relieve pain and reduce swelling (refrigerator temperatures of about 7°).
Warmth
A heat pad can promote blood circulation around the tendons.
Medication
If necessary doctors might suggest that patients take anti-inflammatory drugs for a week or two.
Ointments
Anti-inflammatory creams or ointments can be massaged into the affected site several times a day. This promotes recovery.
Massages
Massages ease muscular tension and relieve pain. Experienced physiotherapists can relax the muscles with just a few massage strokes and increase the blood flow to the targeted area.
Treatment should be adapted to each patient individually to suit his special needs and the exact clinical picture. Patients with postural problems are advised to consult an osteopath.
All-in-one physiotherapy programme for patella tip syndrome
Besides the single-leg squats on a 25° decline board described above, further exercises can be done to stabilise the knee joint and strengthen the patellar ligament in the long term. medi HQ has joined Dr Matthias Marquardt, sports doctor and active sportsman, to compile a training programme. It contains eleven exercises, including the single most important exercise described above, that can be done quickly and simply at home. In the videos, Dr Matthias Marquardt teams up with the professional triathlete and physiotherapist Laura Philipp to show how the exercises are done correctly – ideally three times a week.
Please ask your physio whether the exercises are suitable for you.
Coordination
Exercises on the stabilisation pad are perfect for developing balance and coordination skills. These are best carried out barefoot. The board’s soft foam material makes you sink into the mat a little whilst having to compensate for the resulting instability. This improves proprioceptive skills (proprioception = awareness of the body in space) and strengthens the deeper muscles.
Standing on one leg
Muscles involved: foot and hip muscles
Equipment:
- Stabilisation pad (alternatively: rolled-up towel, folded exercise mat)
Starting position:
- Stand on one leg, barefoot and upright, on the stabilisation pad
- Keep the knee of the leg you are standing on slightly bent
- Lift the other leg up (one-leg stance) (Fig. 1)


Exercise:
-
Lift your free leg and both arms away from your body (Fig. 2)
-
Now slowly bring your arms and your free leg back towards your body (slow "jumping-jack movement")
-
You must thereby permanently compensate for the instability created by the soft surface of the stabilisation pad.
-
This automatically activates your foot and hip muscles
-
Please make sure your trunk muscles are tensed and that you maintain an upright posture
-
To do this, tense your abdominal muscles and make yourself as tall as possible
Variations:
- Make the exercise easier by doing it on a hard surface (without the stabilisation pad)
Jumping Jack
Muscles involved: foot and trunk muscles
Equipment:
- Stabilisation pad (alternatively: rolled-up towel, folded exercise mat)
Starting position:
- Stand on one leg, barefoot and upright, on the stabilisation pad
- Keep the knee of the leg you are standing on slightly bent (Fig. 1)
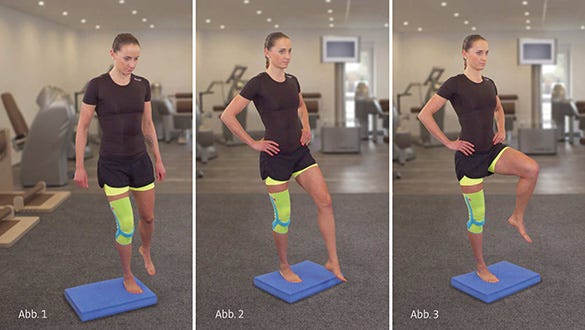
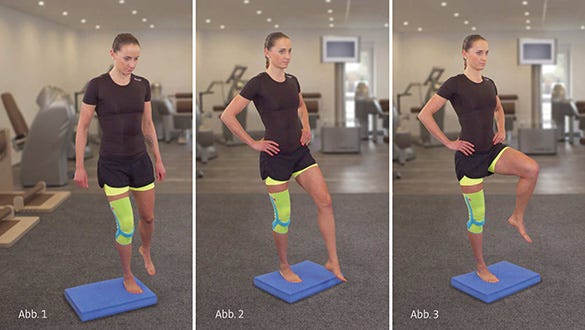
Exercise:
- You must now permanently compensate for the instability created by the soft surface of the stabilisation pad.
- This automatically activates your foot and hip muscles.
- Please make sure your trunk muscles are tensed and that you maintain an upright posture.
- To do this, tense your abdominal muscles and make yourself as tall as possible.
Variations:
- Make the exercise easier by doing it on a hard surface (without the stabilisation pad)
- Make it more difficult by drawing figures of 8 (with the free leg) (Fig. 2)
- Make it more difficult by lifting the free leg up to the hip (Fig. 3)
- Make it more difficult by closing your eyes
Mini knee band
Muscles involved: foot and hip muscles
Equipment:
- Stabilisation pad (alternatively: rolled-up towel, folded exercise mat)
Starting position:
-
Stand on one leg, barefoot and upright, on the stabilisation pad.
-
Keep the knee of the leg you are standing on slightly bent.
-
Stretch out your arms and your free leg as an extension of your upper body and lean forward to an angle of about 20° (Fig. 1).
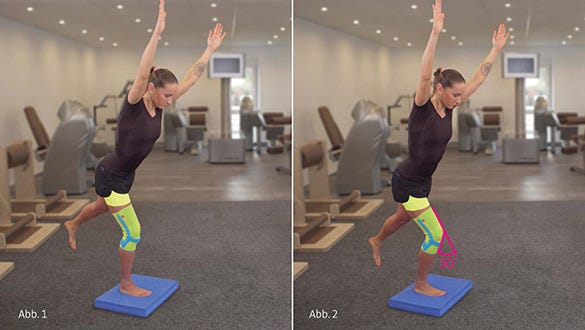
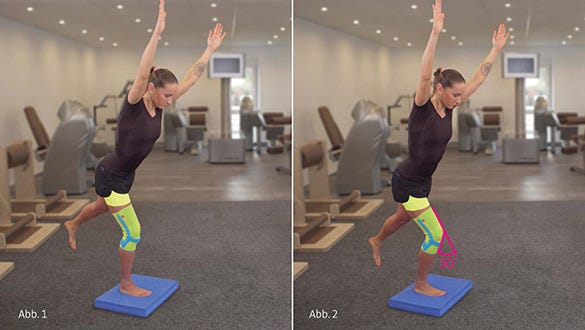
Exercise:
-
Now do "mini knee bends" with the leg you are standing on (to about 30°) (Fig. 2).
-
You must thereby permanently compensate for the instability created by the soft surface of the stabilisation pad.
-
This automatically activates your foot and hip muscles.
-
Your arms, trunk and the lifted leg should form a straight line
-
Please make sure your trunk muscles are tensed
-
Make sure the leg axis is straight
-
Avoid a knock knee position
Variations:
- Make the exercise easier by doing it on a hard surface (without the stabilisation pad)
Dosing:
-
Repeat the exercise 10 times
-
Do three sets on each leg
-
Take a 15 second rest between each of the sets
Strengthening
A dynamic exercise consists of two different movement phases: the eccentric and the concentric phase.
During the concentric (take-off phase, positive-dynamic) phase, a resistance is overcome. In the case of single-leg squats, this would be the knee straightening movement, during which the body weight is pushed upwards. The thigh muscle shortens. The origin and the insertion of the muscle move closer together during the movement. Concentric movements are also often called positive movements.
During the eccentric (relaxing, negative-dynamic) phase, the muscles give way to gravity. In the case of single-leg squats, this would be the knee bending movement, during which the body weight is slowed down (deceleration movement). The thigh muscle is stretched. The origin and the insertion of the muscle move further apart. The muscles stretch under the load. Eccentric movements are also often called negative movements.
Doing eccentric exercises has proved to be particularly successful in the treatment of patella tendinopathy syndrome.
Single-leg knee exercises
Muscles involved: front of the thigh and patellar ligament
Starting position:
-
Stand upright on one leg on a flat, firm surface
-
Keep the knee of the leg you are standing on slightly bent
-
Lift the other leg up (single-leg standing) (Fig. 1)


Exercise:
-
Now do knee bends with the leg you are standing on (up to about 60°)
-
Push your bottom backwards while you do this (Fig. 2)
-
Please make sure your trunk muscles are tensed
-
Do not push your knee ahead of your toes
-
Make sure the leg axis is straight
-
Avoid a knock knee position
-
Do the exercise slowly and under good control
Variations:
-
Make the exercise easier by holding on to something (e.g. a handrail, a therapy rod, broom handle)
-
Make the exercise more difficult by standing on a 25° decline board
Single-leg knee bend with decline boars
Muscles involved: front of the thigh and patellar ligament
Equipment:
- 25° decline board
Starting position:
-
Stand upright on one leg on the 25° decline board
-
Keep the knee of the leg you are standing on slightly bent
-
Lift the other leg up (single-leg standing) (Fig. 1)


Exercise:
-
Now do knee bends with the leg you are standing on (to about 60°) (Fig. 2)
-
Please make sure your trunk muscles are tensed
-
Do not push your knee ahead of your toes
-
Make sure the leg axis is straight
-
Avoid a knock knee position
-
Do the exercise slowly and under good control
Variations:
-
Make the exercise easier by standing on a flat, firm surface
-
Make the exercise easier by holding on to something (e.g. a handrail, a therapy rod, broom handle)
-
Make the exercise more difficult by adding extra weight (e.g. a rucksack with weights)
Lunge
Muscles involved: hamstrings and bottom
Starting position:
-
Stand upright with your feet hip-width apart
-
Do a long backward lunge, so that the heel of the back leg is off the floor
-
Stay upright and keep your back straight (Fig. 1)


Exercise:
-
Keep your back straight, lower the back knee towards the floor and push the front knee forwards (Fig. 2)
-
Now raise your body again a little
-
Then lower the back knee towards the floor again and push the front knee forwards
-
To reinforce the eccentric training, you may push the point of the knee in front of your toes
-
Do the exercise slowly and under good control
Variations:
- Make the exercise more difficult by standing on a 25° decline board
Lunge with decline board
Muscles involved: hamstrings and bottom
Equipment:
- 25° decline board
Starting position:
-
Stand upright with your feet hip-width apart on a 25° decline board
-
Do a long backward lunge with the other leg, so that the heel of the back leg is off the floor
-
Stay upright and keep your back straight (Fig. 1)


Exercise:
-
Keep your back straight, lower the back knee towards the floor and push the front knee forwards (Fig. 2)
-
Now raise your body again a little
-
Then lower the back knee towards the floor again and push the front knee forwards
-
To reinforce the eccentric training, you may push the point of the knee in front of your toes
-
Do the exercise slowly and under good control
Variations:
- Make the exercise easier by standing on a flat, firm surface
Bridging
Muscles involved: hamstrings and bottom
Equipment:
- Exercise mat (alternatively: a towel)
Starting position:
-
Lie on your back
-
Place both heels on the floor (Fig. 1)
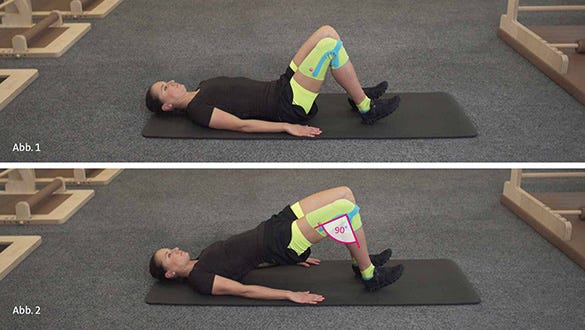
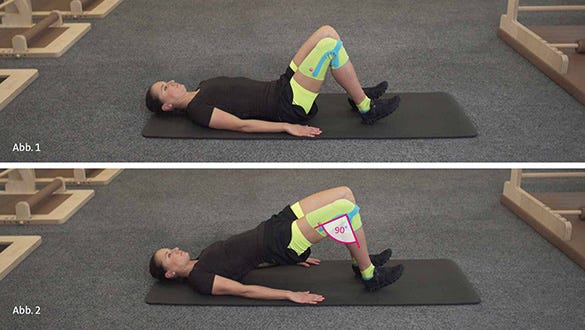
Exercise:
-
Now push your pelvis towards the ceiling
-
Tense your buttocks and pull your tummy button towards your spine (Fig. 2)
-
Now let your pelvis sink back down slowly
-
Then lift your pelvis back up again slowly
-
Please make sure you maintain the right distance between your ankles and your bottom
-
When you have raised your pelvis, your knee bend angle should be 90°
Variations:
- Make the exercise more difficult by performing it on one leg (hold the free leg in the air with the hip and knee bent)
Calf raise
Muscles involved: calf muscles
Equipment:
- A stair tread (optionally with a handrail at the side)
Starting position:
-
Stand with the balls of both feet on the edge of a step (e.g. stair tread)
-
Bend your knees slightly


Exercise:
-
Now push your pelvis towards the ceiling
-
Tense your buttocks and pull your tummy button towards your spine (Fig. 2)
-
Now let your pelvis sink back down slowly
-
Then lift your pelvis back up again slowly
-
Please make sure you maintain the right distance between your ankles and your bottom
-
When you have raised your pelvis, your knee bend angle should be 90°
Variations:
- Make the exercise more difficult by performing it on one leg (hold the free leg in the air with the hip and knee bent)
Dosing:
-
Repeat the exercise 10 times
-
Do three sets (single-leg variant: three sets per leg)
-
Take a 30 second rest between each of the sets
Stretching & fascia training
Stretching and fascia training can ease the tension on the painful patellar ligament. Fasciae are connective tissue structures that surround and stabilise the muscles. A fascia roller stimulates the circulation to the tissues to improve tissue tone.
Iliopsoas muscle
Muscle involved: iliopsoas muscle
Equipment:
- Exercise mat (alternatively: a towel)
Starting position:
-
Stand in a long lunge position
-
Rest your back knee on the floor ("dubbing" position)
-
Stay upright and keep your back straight (Fig. 1)


Exercise:
-
Press your hips forwards with your hands until you sense a feeling of tension in the groin (Fig. 2)
-
Please be sure not to push the point of the knee in front of your toes
-
If you find the pressure on your kneecap uncomfortable, you can use a softer surface.
Dosing:
-
Roll backwards and forwards 10 times
-
Do three sets (single-leg variant: three sets per leg)
-
Take a 30 second rest between each of the sets.
Front of the thigh
Muscles involved: front of the thigh
Equipment:
- Exercise mat (alternatively: a towel)
Starting position:
-
Lie on your side on the floor
-
Bend both the knee and the hip of the lower leg to an angle of 90° (Fig. 1)
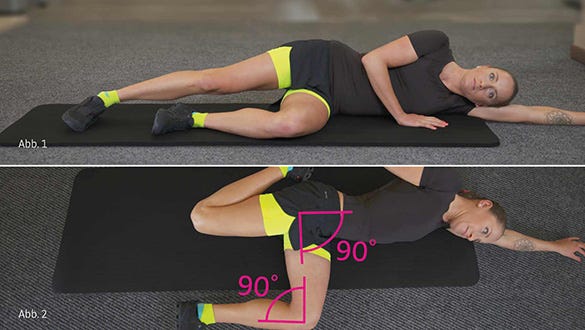
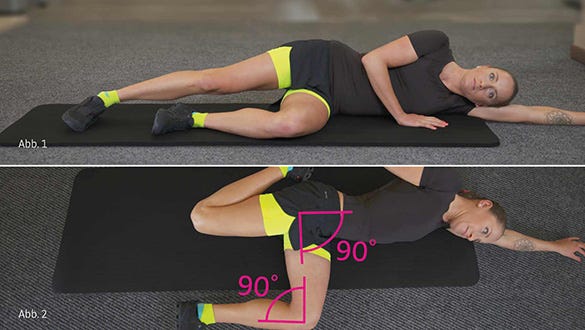
Exercise:
-
Now pull the upper leg backwards by grasping your ankle joint until you feel the stretch down the front of the thigh (Fig. 2)
-
Please make sure you keep your thigh parallel to the floor.
-
Always tense your abdominal muscles and avoid a hollow back.
Thigh rolling
Muscles involved: muscles over the front of the thigh
Equipment:
- Fascia roller (e.g. from Blackroll®)
- Optional: exercise mat
Starting position:
-
Lie on your front
-
Place the massage roller under the muscles over the front of your thigh
-
Lean on your forearms (Fig. 1)


Exercise:
-
Roll backwards and forwards over the roller slowly along the full length of the front of your thigh, i.e. from your knee to the hip.
-
You will feel the pressure point treatment in the muscles over the front of your thigh (Fig. 2).
-
Keep your trunk straight and relax the muscles over the front of the thigh – as far as possible.
-
The exercise may be slightly painful at first, but the pain should never be more than you can easily tolerate.
Calf rolling
Muscles involved: calf muscles
Equipment:
- Fascia roller (e.g. from Blackroll®)
- Optional: exercise mat
Starting position:
-
Sit on the floor
-
Place one foot on the floor and lay the calf of the other leg on the fascia roller
-
Lean back on your hands (Fig. 1


Exercise:
-
Lift your bottom a little off the floor.
-
Now slowly roll the whole length of your calf, forwards and backwards, i.e. from the Achilles tendon to the hollow of the knee.
-
You will now feel the pressure point treatment in your calf muscles.
-
Your trunk muscles will help move your body (Fig. 2).
-
Point your toes downwards, so that your calf muscles are relaxed.
-
The exercise may be slightly painful at first, but the pain should never be more than you can easily tolerate.
Variations:
- Make the exercise more difficult by rolling both legs
- Make the exercise more difficult by crossing your legs
medi has developed the knee support Genumedi PSS for conservative therapy of patellar tendinopathy. It combines the tried-and-tested properties of a support with the additional benefit of a patellar support strap: the support safely and reliably guides and stabilises the knee joint and relieves tension on the insertions of the patellar ligament.






